Von Willebrand Disease: A Comprehensive Guide

Von Willebrand Disease (VWD) is a hereditary bleeding disorder caused by a deficiency or dysfunction of von Willebrand factor (VWF), an essential protein for blood clotting. This blog explores its types, causes, symptoms, and treatment options, providing a deeper understanding of how to manage this condition effectively.
What is Von Willebrand Disease?
To begin with, Von Willebrand Disease is a genetic condition that impairs blood clotting. It occurs due to a deficiency or defect in von Willebrand factor, a protein critical for clot formation. Consequently, individuals with this condition may experience prolonged bleeding after injuries or surgeries.
Types of Von Willebrand Disease
Type 1
- Description: This is the most common and mild form of VWD.
- Cause: Partial deficiency of von Willebrand factor.
- Symptoms: Individuals often experience mild bleeding, including frequent nosebleeds or prolonged bleeding from minor injuries.
Type 2
- Description: This type includes subtypes (2A, 2B, 2M, 2N) and involves defects in the quality of VWF.
- Symptoms: Bleeding severity varies among subtypes.
- Note: Although VWF levels may be normal, the protein functions improperly.
Type 3
- Description: Rare and severe, this form results from little to no production of von Willebrand factor.
- Symptoms: Patients often experience severe bleeding episodes, including joint and muscle bleeding.
Von Willebrand Syndrome vs. Von Willebrand Disease
Interestingly, while the terms “Von Willebrand Disease” and “syndrome” are often used interchangeably, they refer to different conditions. Von Willebrand syndrome describes acquired forms of VWD, which arise from other medical conditions, such as autoimmune diseases or certain cancers, rather than genetic inheritance.
Symptoms
For those with VWD, the following symptoms are common:
- Frequent and prolonged nosebleeds.
- Heavy or long menstrual periods.
- Easy bruising.
- Blood in urine or stool.
- Bleeding gums after dental work or brushing teeth.
Severe Symptoms (Type 3)
However, in severe cases like Type 3, symptoms may include:
- Swelling in joints due to internal bleeding.
- Significant bleeding after minor injuries or medical procedures.
Diagnosing Von Willebrand Disease
Steps in Diagnosis
To diagnose VWD, physicians typically follow these steps:
- Medical History: They review family history for evidence of bleeding disorders.
- Physical Examination: A detailed check for visible bruises and other bleeding symptoms is conducted.
- Laboratory Tests:
- Von Willebrand Factor Antigen Test: Measures VWF levels.
- Ristocetin Cofactor Activity Test: Assesses VWF’s platelet-binding capacity.
- Factor VIII Activity Test: Evaluates clotting ability, often reduced in VWD.
- Genetic Testing: Confirms mutations in specific cases.
Notably, these tests help determine the type and severity of VWD, guiding effective treatment plans.
Treatment for Von Willebrand Disease
Mild to Moderate Cases (Type 1 and Type 2)
For most individuals with mild or moderate VWD, the following treatments are effective:
- Desmopressin (DDAVP): This synthetic hormone stimulates VWF release from blood vessel linings.
- Antifibrinolytic Drugs: Often used during dental procedures, these drugs prevent clot breakdown.
Severe Cases (Type 2 and Type 3)
In contrast, severe cases require more intensive treatments, including:
- VWF Replacement Therapy: Infusion of VWF concentrates to manage bleeding episodes.
- Plasma Therapy: Used in emergencies or when other treatments are ineffective.
Other Supportive Treatments
Moreover, additional supportive treatments include:
- Birth Control Pills: These help reduce heavy menstrual bleeding.
- Topical Agents: Promote clotting when applied directly to wounds.
Living with Von Willebrand Disease

Managing Symptoms
Living with VWD can be challenging, but managing symptoms effectively can make a significant difference. For example:
- Avoid medications like aspirin and NSAIDs that worsen bleeding.
- Use protective gear during physical activities to minimize injury risk.
- Schedule regular check-ups with a hematologist.
Lifestyle Tips
Furthermore, adopting certain lifestyle practices can help improve quality of life:
- Maintain a balanced diet and healthy weight to support overall well-being.
- Practice good dental hygiene to prevent gum-related bleeding.
- Wear a medical alert bracelet to inform first responders about the condition.
Conclusion
In conclusion, Von Willebrand Disease, while challenging, is manageable with timely medical intervention and lifestyle adjustments. By raising awareness and ensuring access to effective treatments, individuals with VWD can lead fulfilling lives. If you suspect VWD in yourself or a family member, consult a healthcare provider for proper diagnosis and management.
For more information: World Federation of Haemophilia (WFH): Global insights into Von Willebrand Disease are available at WFH.org. American Society of Hematology (ASH): Access expert-reviewed research and treatment options at Hematology.org.
FAQs
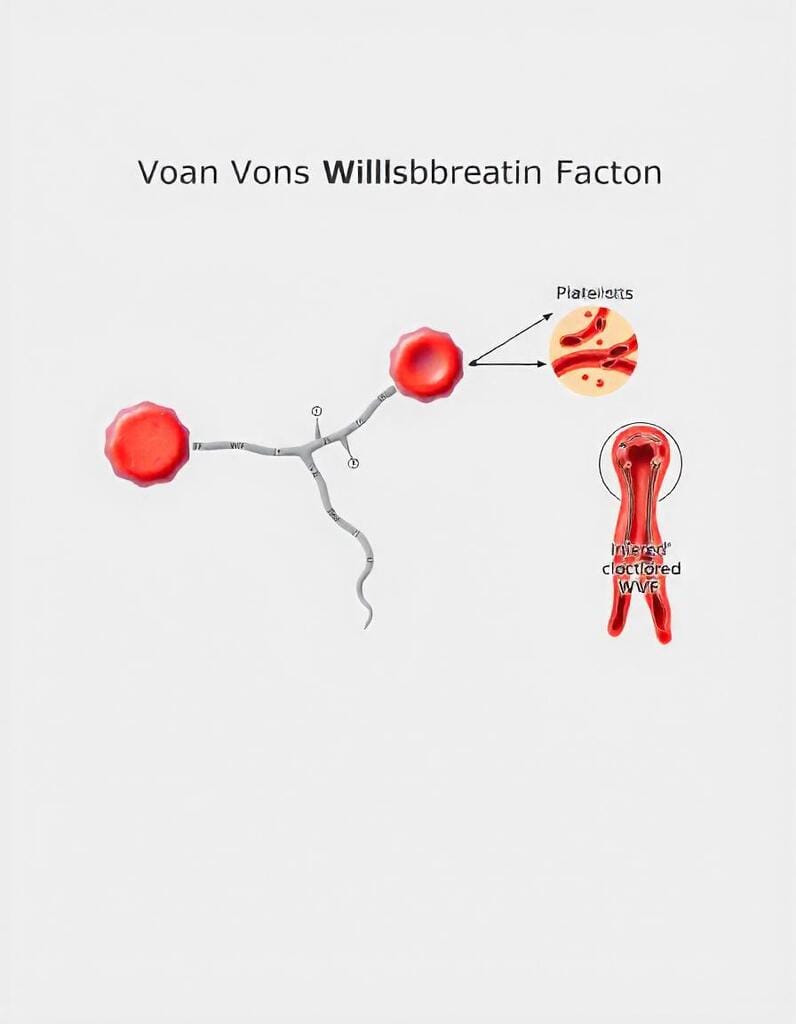
What is Von Willebrand Factor?
Von Willebrand factor is a protein essential for helping blood platelets adhere to each other and vessel walls during clot formation.
What Causes Von Willebrand Disease?
It is primarily a genetic condition, passed through autosomal dominant or recessive inheritance.
Can Von Willebrand Disease Be Cured?
Unfortunately, there is no permanent cure. However, modern treatments help manage symptoms effectively.
How is VWD Different from Hemophilia?
Although both involve bleeding disorders, VWD is caused by VWF defects, whereas hemophilia involves factor VIII or IX deficiencies.
What Are the Risks of Untreated VWD?
If left untreated, individuals may suffer severe bleeding, joint damage, and complications during surgeries or childbirth.
